- The eBay Community
- Groups
- Fun & Social
- Community Spirit
- Re: State by State, Australia vs Elsewhere, in the...
- Subscribe to RSS Feed
- Mark Topic as New
- Mark Topic as Read
- Float this Topic for Current User
- Bookmark
- Subscribe
- Mute
- Printer Friendly Page
State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 20-10-2021 08:12 PM
This thread is for the specific purpose of checking on milestone information (quotations and videos rather than table-form/spreadsheet/database information that fit better into k1ooo's thread), and responses by representatives from our government, CHOs, etc.
It's official: Australia has passed the 70% double dose vaccination rate.
❝Australia's double-dose vaccination rate has passed 70 per cent of all adults aged 16 and over
It is a key milestone in the national reopening plan.
More than 33 million vaccine doses have been distributed nationwide, and the first-dose rate nationally has reached 85.5 percent.
New South Wales and the ACT have already passed the 80 percent vaccination milestone, and Victoria and Tasmania are expected to reach 70 percent double-dosed within two days.❞
A tremendous achievement, but of course there is still some patchiness. We'll have to see some good efforts to correct misinformation, to provide solid health information, and to take the vaccine to the people who are not able or not willing to access it easily by themselves.
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 16-11-2021 11:57 PM
That’s enough of a meander, please.
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 17-11-2021 01:28 PM
I wonder what the going rate is
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 17-11-2021 01:42 PM
my ears are burning !
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 17-11-2021 01:57 PM
The vaxxed should be tested for coronavirus antigen activity 2 weeks later to ensure effectiveness and also to ensure no fudging by conscientious objectors who have been left with no alternatives
btw although maybe c.o's should be eligible for an exemption - we do so in times of conflict .
also if one has recovered from a clinically confirmed bout of covid one is by definition immune so should be qualified for an exemption = what is the point except being a convenient object of government generic population pandemic management . Jab everyone and then no enforcement systems required ( sort of like universal wage )
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
17-11-2021 02:17 PM - edited 17-11-2021 02:18 PM
None of the vaxxed should met coronavirus related untimely deaths
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
17-11-2021 04:04 PM - edited 17-11-2021 04:04 PM
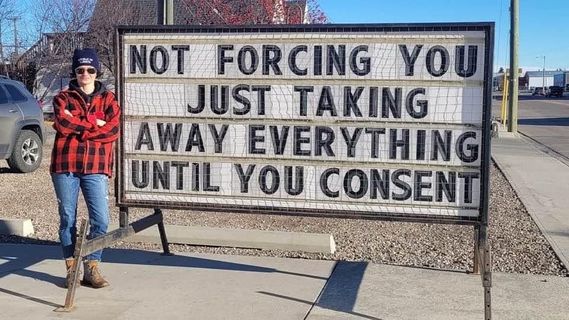
Not sure at this point if I am on topic or not, but the Vax is NOT truly voluntary any more and is as close to mandatory as it can get.
Myslef and my three family members all had to be vaxxed or not work as from 17 November - so to support ourselves and our respective families we were given NO choice - if that is not Mandatory, I don't know what it is.
I am not in the for or against camp - my beliefs are my own and not for public consumption, but those that still beleive this is a "voluntary vax choice" - just wait......
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 17-11-2021 04:21 PM
You - answered me.
@rogespeed wrote:The vaxxed should be tested for coronavirus antigen activity 2 weeks later to ensure effectiveness and also to ensure no fudging by conscientious objectors who have been left with no alternatives
Please explain - seems I'm thick.
btw although maybe c.o's should be eligible for an exemption - we do so in times of conflict .
Please explain - seems I'm thick.
also if one has recovered from a clinically confirmed bout of covid one is by definition immune so should be qualified for an exemption = what is the point except being a convenient object of government generic population pandemic management . Jab everyone and then no enforcement systems required ( sort of like universal wage )
Where have you been - if one has recovered from a clinically bout of Covid - one is - BY DEFINITION - NOT IMMUNE.
Covid can be contracted - yet again - transmitted - yet again - and - yet again.
Between you & the other - it's a hard row to plow. 😂
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 17-11-2021 07:19 PM
I'm re-posting the letter/editorial sent by Brett Sutton and Stephen Duckett to the AMJ, as I think it's somehow got lost among the repeated posts here that are arguing against the vaccine, against mandated vaccines, and for unproven treatments.
There really are so many other threads for those discussions, so could I ask again that this thread remain on-topic? Discussion about milestones and information released by our government (Federal and state) officials, in particular our Health Officers would fit in here perfectly.
From the Medical Journal of Australia
EDITORIAL
On entering Australia’s third year with COVID‐19
Stephen J Duckett and Brett Sutton
Med J Aust || doi: 10.5694/mja2.51328
Published online: 15 November 2021
We cannot let complacency encumber how we live with the virus: vigilance and a planned recovery are essential
In 2022, Australia will enter its third year with COVID‐19, the coronavirus disease caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). If 2020 was characterised by the fight for “COVID‐zero”, and 2021 by the drive to vaccinate Australia, 2022 and beyond could be the start of the inter‐pandemic period: if all goes well, community vaccination levels will be high enough that the occasional COVID‐19 outbreak will not require lockdowns or other strict public health measures.
The caveat concerns the nature of the virus. All viruses mutate, new dominant strains emerge. We do not know whether the next SARS‐CoV‐2 strain will be nastier than its predecessor, or whether a new vaccine will be required and could be developed quickly. At this stage, we also still don’t know whether everyone will need booster vaccination shots or whether lessons learned during the messy 2021 vaccination program will improve the management of their rollout.
But the 2022‐and‐beyond vaccine program is but one of the policy challenges Australia needs to consider. More broadly, all governments need to be involved in planning the recovery phase, to ensure that they can manage the impact on health systems and protect public health during the inter‐pandemic period.
The missing recovery phase
The National Cabinet COVID‐19 roadmap (released in July 2021) ends with the “final post‐vaccination phase”, which includes border re‐openings and living with COVID‐19 in the community without lockdowns.¹ Disappointingly, the roadmap includes no explicit recovery phase: it [is] as if we could all soon heave a sigh of relief and simply move on.
The recovery phase after public health emergencies normally includes addressing their economic effects and managing the mental health impacts.² COVID‐19 became a disease of low income workers — those who couldn’t work from home — and their families and communities. It affected Australia very unevenly, with poorer outcomes for those at greatest disadvantage.³ The recovery phase needs to rebuild community and system resilience and redress disadvantage exacerbated by COVID‐19. Planning for workforce responses, especially preparing for burnout and the needs of staff for time out to recover, will be critical. It should also include governments, hospitals, and primary care services learning from the crisis: what went well, what went badly? From a public health perspective, this should not be a witch hunt, but rather an exercise in learning and improvement. The learning process should be undertaken at both local — what were the changes, what was their impact and cost, what did staff and patients think about them? — and at state and national levels, including formal inquiries.
Health system lessons
The Australian health system adapted remarkably well during the acute phase of the pandemic. Hospitals responded very flexibly, boosted hospital‐in‐the‐home services, and expanded telehealth options for outpatient clinics. General practitioners also embraced telehealth. Hospitals established mass vaccination hubs rapidly, and managed them well. But all was not perfect. Staff were under enormous pressure, and symptoms of limitations to hospital capacity were evident in most states.
2022 will bring new challenges. The continuing mental health effects of disruptions to life during 2020 and 2021 are already being seen in the health system, and, as with natural disasters, they will need to be managed for years, not weeks.⁴ Deferred care (system‐deferred, such as elective procedures, or patient‐deferred, including care missed because patients with troubling symptoms postponed seeking help) will need to be resumed. “Long COVID” is also a serious and, to some extent, still undefined phenomenon.⁵,⁶ The reporting of some signs, such as parosmia (for which there is currently no effective treatment), has increased dramatically.⁷ The long term effects of COVID‐19 on cardiac and respiratory function are still being assessed. Health services will need to plan for staff who need to recover from COVID‐19‐induced burnout.⁸
Decision makers in health systems will need to spend early 2022 assessing and developing strategies in response to these problems, and this situation will be more confronting if new vaccine‐resistant virus variants emerge, or the effectiveness of current vaccines wanes.⁹,¹⁰ The federal government will need to finalise a policy on permanently incorporating telehealth into primary care and specialist care in the community. It also needs to share the increased health care costs caused by the pandemic; and not just the direct costs, which it has already agreed to share with the states on a 50:50 basis, but also the costs of deferred care in 2022 and possibly even 2023. Under current arrangements, these costs will be borne entirely by the states because of the cap on federal funding.
Public health during the inter‐pandemic period
Public health is the art and science of protecting and improving the health of people and communities by promoting healthy behaviours, workplaces, and communities, and preventing or responding to communicable and non‐communicable environmental and lifestyle diseases and other hazards. In 2022, public health will need to concern itself with the emerging burden of disease and avoidable harms linked with the profound effects of the COVID‐19 pandemic over the past two years.
The real lesson of the pandemic, however, is the huge impact of inequality and structural disadvantage on its course and outcomes. It is convenient to imagine that respiratory viruses are randomly transmitted from one person to another. The reality is that they find all the social, demographic, and economic vulnerabilities within and between populations: differential effects related to sex, overcrowding, essential but casualised work, public housing, homelessness, poverty, poor health literacy, cultural marginalisation, and stigmatisation. These are not individual human behavioural problems as much as “causes of the causes”.¹¹,¹²
Such fundamental disparities across the social spectrum apply as much to non‐communicable disease as to pandemics: we see it in inequitable health outcomes during extreme heat, in congenital syphilis, and in people exposed to environmental hazards, such as poor air quality. COVID‐19 vaccination rates have been much lower for First Nations people than other Australians, despite their priority status during stages 1b and 2a of the vaccine rollout,¹³ and are at greater risk of both transmission and severe illness if infected.¹⁴
In 2022, public health practitioners and organisations must seek to better understand these social drivers of health in the COVID‐19 era, and receive the resources to redress disparities exacerbated by the crisis. How has prolonged remote learning affected children and communities differently? How have young people fared, a group particularly exposed to mental health problems, loss of employment, and casual work hours? And how can they best be helped in the years ahead?
Conclusion
Australia weathered the COVID‐19 storm well. Our death rate was among the lowest in the world, and the impact on the economy was also relatively mild. But these successes may have hindered our vaccination rollout. We cannot allow complacency to similarly encumber how we live with COVID‐19. We must be vigilant, to ensure that our first‐rate public health capacity is not run down as part of public sector belt tightening. We must ensure that our health system has the capacity to respond to the shadow pandemic of mental health problems caused by the viral pandemic and its management,¹⁵ and that we are well placed to face the challenges of both long COVID and future pandemics.
My brief comment: The Victorian CHO Brett Sutton and Stephen Duckett make some powerful points. In particular, managing the long term effects of COVID-19 would seem to merit a recovery phase, and there is room for discussion about bearing ongoing costs and putting into place the lessons learned so far. At any rate, I thought it was an interesting read.
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 17-11-2021 07:44 PM
I haven't read the thread, but most of the country is well over 80% double-stabbed. Where I live it's pushing 97% of 12+. Which should be the measure every state uses.
The states that are lagging are those that didn't push vaccination in the first place. Hopefully they will incur the economic costs (the only language governments understand).
As far as 'recovery' goes, the vaccines don't give immunity, but they DO reduce the virus load, and thus the chances of infecting others.
A bit like all the other flu strains out there.
Re: State by State, Australia vs Elsewhere, in the age of COVID-19 and beyond
- Mark as New
- Bookmark
- Subscribe
- Mute
- Subscribe to RSS Feed
- Highlight
- Report Inappropriate Content
on 18-11-2021 10:21 AM